|
|
|
|
|
|
||||||

| Home | About Us | Sitemap |
|
|
|
|
|
|
Nerve conduction study (NCS) and electromyography (EMG) are useful techniques to evaluate the localization and pathophysiology of sensory and motor dysfunction in patients seen by neurosurgeons. These techniques are an extension of the clinical history and physical examination and must be designed and interpreted concurrent with that information. The tests are subject to technical error, so familiarity with the quality of the study performed in the EMG laboratory is crucial to the clinician's confidence in the results. When the referring neurosurgeon requests the study to answer a specific clinical question or queries whether electrophysiologic techniques could be helpful in the assessment of his or her patient, direct communication with the electromyographer is useful. When patients with hepatitis, Creutzfeldt-Jakob disease, or HIV-related disease are scheduled for EMG, the laboratory should be notified for their protection and handling of equipment. Other clinical information, including pacemaker use, central line placement, neutropenia, and coagulation status, may also influence the way the study is performed and should be communicated. Children can be evaluated by NCS/EMG. Young children are usually sedated for the NCS and awake but drowsy for the EMG. These studies may be helpful in evaluating floppy infants and children with traumatic brachial plexopathy or other neuromuscular complaints. Here is a basic introduction to how NCS and EMG are performed as well as how the data can be useful to the neurosurgeon. Suggested criteria for the design of appropriate NCS/EMG studies for a given clinical situation have been published but need to be individualized based on the patient's history and physical findings.
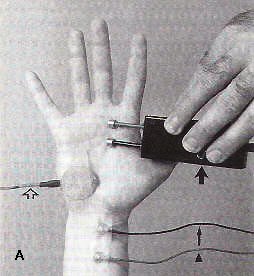
Orthodromic conduction sends impulses in the same direction as physiological conduction. i.e., toward the spinal cord for sensory conduction and to muscle for motor conduction. Antidromic conduction is in the reverse direction. Sensory complaints can be evaluated by a sensory NCS. A supramaximal stimulus is delivered to a sensory nerve and the orthodromic response is recorded, often by a surface electrode placed over the course of the nerve at a fixed distance from the stimulation site (Fig-1A).
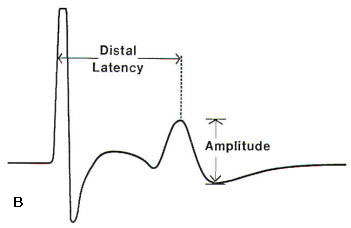
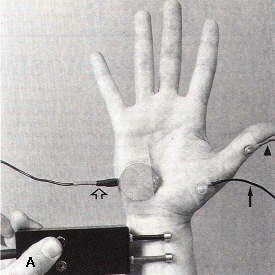
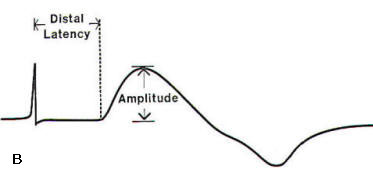
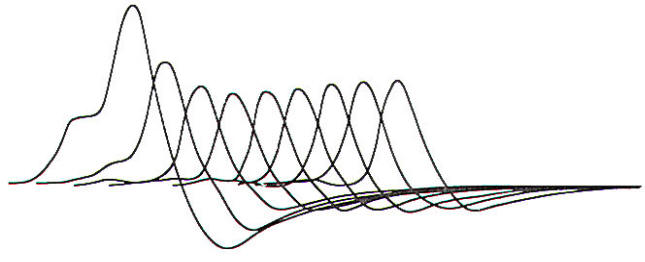
The speed of conduction of both sensory and motor fibers is determined by the integrity of heavily myelinated fibers and the preservation of saltatory conduction between individual nodes of Ranvier. If the myelin is disrupted between the stimulus and recording sites, the recorded potential will be delayed in onset. This measurement is called the distal latencv and in sensory conductions is the time from the stimulus onset to the peak of the sensory nerve action potential (SNAP) (Fig-1B). Conduction velocity in sensory nerves is calculated by dividing the measured distance between the stimulation and recording sites by the distal latency. With a supramaximal stimulus, all of the axons beneath the stimulator should depolarize, resulting in a waveform amplitude commensurate with the number of underlying axons depolarized. The amplitude is measured from the peak to the trough of the SNAP (Fig-1B). Each EMG laboratory should have normal values with controls for patient age and height. Skin temperature should be controlled, which may require warming the limb. These factors can significantly affect the results of the conduction studies. Technical errors such as not placing the recording electrode directly over the nerve being tested or not achieving supramaximal stimulation of the nerve can artificially lower the amplitude of the SNAP. Factors such as inaccurate distance measurements or a cold limb can markedly alter distal latency and conduction velocity determinations. Motor NCSs can aid in the assessment of the etiology of weakness. A recording surface electrode is placed over the belly of the muscle being studied (Fig-2A). Through orthodromic, supramaximal stimulation of the motor nerve at a fixed distance, a waveform called the compound motor action potential (CMAP) is obtained (Fig-2B). This waveform represents the summation of the depolarization of muscle fibers beneath the recording electrode. This distal latency is determined by recording the time from the stimulus onset to the initial motor response. The motor nerve is then stimulated from a second, more proximal site and a second CMAP is obtained. The conduction velocity of the nerve segment between stimulation sites is calculated by dividing the distance between stimulation sites by the difference between distal latencies. In motor nerves such as the ulnar or peroneal nerve that are commonly susceptible to compression about fixed structures, a third stimulation site is used to span the possible compression site. The conduction velocity can then be calculated from each of the two proximal sites and compared. Focal slowing of more than 10 m/s in a short segment is considered significant. With supramaximal stimulation of the motor nerve, all motor fibers beneath the stimulus are depolarized, resulting in a maximal contraction of the muscle being recorded. The amplitude of the CMAP is thus dependent on the state of the motor axons. Amplitude is measured from the baseline to the peak of the CMAP. However, other processes besides axonal failure can result in a low CMAP amplitude. If muscle mass is decreased from any cause such as a previous central nervous system injury or malnutrition, the CMAP amplitude can be lowered. Also, severe myopathy or neuromuscular junction disease can result in a low CMAP amplitude. EMG is thus needed to clarify the cause of the low CMAP amplitude. The area of the CMAP correlates with the amplitude and may better reflect the amount of muscle being depolarized. Evaluating the amplitude and degree of dispersion of the CMAP can greatly assist in understanding the underlying pathophysiology of the nerve lesion. Neurapraxia refers to nerve conduction failure without axonal loss and implies a demyelinating lesion. If enough fibers fail to conduct impulses because of conduction block across a given segment, the CMAP amplitude will decrease during nerve stimulation proximal to the block; 25 to 30 percent is a significant degree of change in most nerves. Focal slowing affecting fast conducting fibers will delay the CMAP. If there is differential slowing of slow conducting fibers along a nerve segment, the CMAP waveform will be dispersed, thus demonstrating a desynchronization of fiber firing. Motor NCSs are difficult technically and errors may result from improper placement of electrodes, incorrect measurements, or submaximal stimulation. Once again, height, age, and skin temperature are important. Another parameter that can be measured to evaluate conduction along a motor nerve is the F-wave, one type of late response. This response is obtained with supramaximal stimulation while motor conduction studies are being performed. When a nerve is stimulated there is depolarization of that nerve in both directions. The F-wave response is caused by recurrent firing of the anterior horn cell after antidromic conduction. Therefore both the afferent and efferent limbs of this response are motor. Because this response evaluates proximal nerve conduction, it can be useful in evaluating patients for root or plexus injury. It may be especially useful in the acute stage before evidence of peripheral nerve degeneration and denervation changes (as detected by EMG) has developed. Because of the length of nerve traveled by the impulses, normal values are different based on the subject's height. F-wave latencies are determined by analyzing at least 10 F-waves and recording the earliest latency. Another type of late response, the H-reflex, is different from the F-wave in that the afferent limb of the H-reflex is sensory and the efferent limb is motor. The H-reflex is tested by stimulating the tibial nerve in the popliteal fossa and recording from the gastrocnemius muscle. The H-reflex afferent limb is through the S1 root. Responses are determined with submaximal stimulation and are compared to the responses on the contralateral side. An asymmetry of 2 ms is considered significant. Normal patients may have bilaterally absent H-reflexes so that bilateral absence of response is not necessarily pathologic. Both F-wave latency and H-reflexes are most useful when peripheral conduction studies are normal; abnormal responses suggest a proximal lesion. However, when routine motor conduction is abnormal, abnormality of these late responses may not necessarily be indicative of a proximal lesion. After nerve injury, such as with a remote history of a radiculopathy, late responses may remain abnormal indefinitely. Therefore the interpretation of an abnormality would benefit from comparison with a previous study. To summarize, distal latency and conduction velocity measurements are particularly helpful in evaluating the speed of conduction along distal and mid-portions of a peripheral nerve, respectively. The F-wave latency is particularly useful in evaluating conduction along proximal segments of a motor nerve if the distal segments are normal. When the electromyographer uses the term demyelinating features. reference is made to prolonged distal latency, slow conduction velocity, prolonged F-wave latency, or dispersed waveforms. The amplitude of the CMAP is altered by failure of conduction to the muscle and the waveform may be helpful in understanding the reason for the altered conduction. Axonal features usually imply low amplitudes. However, an EMG study of the muscle is needed to clarify the reasons for a low CMAP amplitude. Both sensory and motor conduction studies are highly reproducible, although there is better intra-examiner reliability than inter-examiner reliability. Conduction studies are focused on an area of clinical abnormality; distant areas are studied also, to classify the abnormality as focal, multifocal, or diffuse. In studies in which a focal conduction block is suspected but not definitely proven by the routine studies, a technique called inching can be used. The region of the suspected block is studied by nerve stimulation above and below the presumed site of the block at 1-cm intervals searching for a focal dramatic change in distal latency. These studies are frequently useful in the evaluation of a suspected carpal tunnel syndrome, ulnar neuropathy at the elbow, and peroneal neuropathy at the knee.
Blink responses, like the corneal reflex, allow evaluation of trigeminal sensory and facial motor conduction. Surface electrodes are placed on the orbicularis oculi muscles bilaterally, along with surface reference electrodes and a ground. Stimulation of the supraorbital nerve or a glabellar tap results in an ipsilateral response via a pontine pathway through the main sensory trigeminal nucleus and the facial nucleus. The response is designated R1. Thus, this R1 response evaluates trigeminal and facial nerve conduction. Subsequent to the R1 response is a second bilateral response, designated R2, that is polysynaptic and more diffuse in brain stem localization. The RI response is best used for evaluating conduction velocity along the trigeminal and facial nerves because it is a shorter reflex. The R2 response is best used in localizing the lesion to right or left trigeminal or facial nerves. These studies along with routine motor conduction studies of the facial nerve and EMG of the facial muscles may be useful in analyzing several disorders affecting the facial and trigeminal nerves.
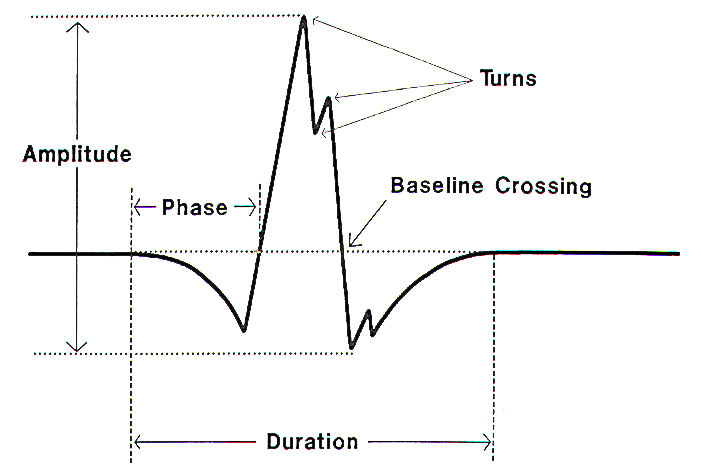
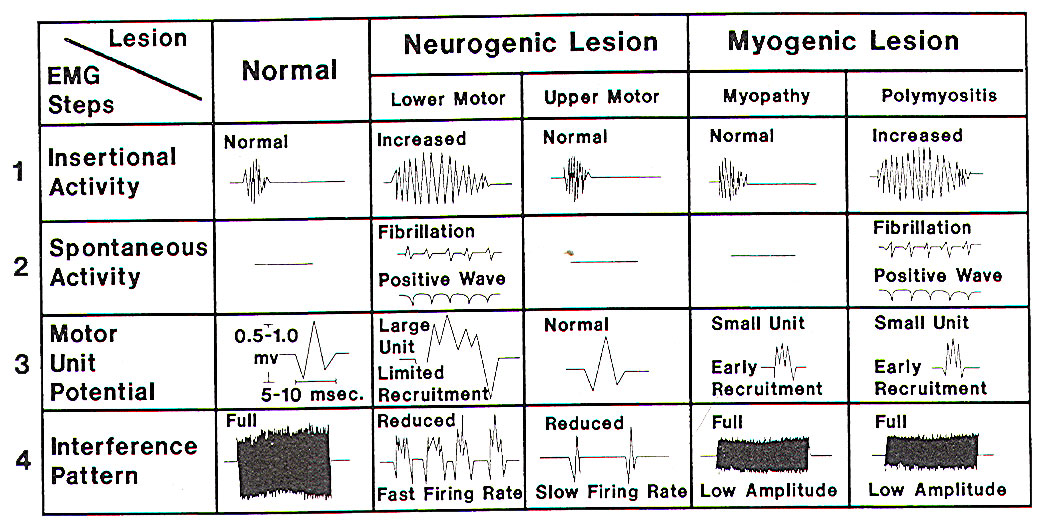
Electromyography is an important procedure in the evaluation of lower motor neuron dysfunction. A needle electrode is placed into the muscle being studied and potentials are evaluated visually on an oscilloscope and audibly. Several different types of needle electrodes can be used and each has particular recording characteristics. Contraindications to this procedure include active cutaneous infection at the site of insertion and absolute neutropenia. Patients with a coagulopathy should be examined with caution. Normal muscle is silent at rest. The first parameter evaluated during the EMG is called insertional activity. Normal insertional activity occurs during movement of the needle in the muscle secondary to the mechanical discharge of muscle fibers. It is diminished when the muscle is fibrotic or edematous and increased when fibers are hyperirritable as in an inflammatory myopathy or denervated muscle. Each muscle tested is usually examined in four quadrants with five needle movements in each quadrant. After the needle is moved it is left at rest and spontaneous activity is evaluated. Spontaneous firing of individual muscle fibers occurs when the fibers are functionally denervated. This can be due to a neurogenic process, myopathy or severe neuromuscular junction disorder. The spontaneous activity is seen as fibrillations or positive sharp waves. A fibrillation is the action potential from a single muscle fiber and is usually a very short, biphasic potential of low amplitude. Positive sharp waves are recorded from a single muscle fiber and are small downward deflections on the oscilloscope. The relative amount of spontaneous activity seen can be scored on a 1 to 4 system (Table -1). After acute denervation with axonal injury, spontaneous activity can be delayed in appearance for 10 to 14 days. The closer the site of denervation to the muscle examined, the earlier denervation changes can be seen. An EMG study immediately after a nerve injury may not show denervation in the muscles examined even though the muscles are weak.
Fasciculations represent the spontaneous firing of a single motor unit. A motor unit consists of the anterior horn cell, its nerve processes, and the neuromuscular junctions and muscle fibers innervated by that anterior horn cell. Fasciculations can be seen clinically as well as during EMG. The pathologic significance of fasciculations is determined by the clinical and electromyographic findings. If the clinical examination and the remainder of the EMG are normal, fasciculations are termed benign. Pathologically, they are seen most frequently with motor neuron disease but can be seen in other denervating conditions and rarely myopathic processes. Myokymic discharges are the electrical correlate of myokymia seen on examination and appear as bursts of high-frequency discharges at regular intervals on the oscilloscope. Facial myokymia is most often seen in multiple sclerosis or with brain stem neoplasms. Peripheral root, plexus or nerve injury can also cause myokymia. The presence of myokymia may be very helpful in the evaluation of plexopathies in cancer patients because it is more commonly seen in radiation plexopathy than carcinomatous plexopathy.
Another parameter evaluated during the needle study is the interference pattern. This represents the amount of MUPs firing during maximal contraction and can be diminished in any central or peripheral cause of weakness as well as through patient noncompliance. Early in motor neuron disease. the interference pattern is often diminished despite good patient effort. Early in a myopathy. however, the interference pattern is usually full. Fig-5 summarizes the EMG findings in normal subjects and in patients with neurogenic or myogenic disorders.
More sophisticated EMG techniques are available to quantify abnormalities of motor unit potential configuration and recruitment but these techniques are not usually needed in the evaluation of patients most often referred to the neurosurgeon. Single-fiber EMG is a technique that uses a smaller needle electrode in order to better define the complexity of motor unit potentials and the jitter between fibers. Jitter is defined as the interpotential interval between the discharge of two fibers belonging to the same motor unit. In a normal motor unit any two muscle fibers will fire with little variation in time. In a motor unit where there is an abnormality of neuromuscular junction transmission, this interval between firing of individual muscle fibers can increase and be variable (increased jitter). If transmission is totally blocked, the second muscle potential may be absent. This technique is the most sensitive electrophysiologic test in evaluating patients for such primary disorders of the neuromuscular junction as myasthenia gravis or the Lambert-Eaton myasthenic syndrome. It is most sensitive when testing a clinically weak muscle but can be abnormal in clinically normal muscles. Evaluating motor unit potentials for jitter is also done by the electromyographer during routine EMG by visual and auditory inspection of the motor units. Thus, significant abnormalities of neuromuscular junction transmission may be suggested during careful analysis of the motor unit potential during routine EMG.
There is a wide variety of electrophysiologic tests performed to evaluate autonomic function. Frequently. the RR interval variation on electrocardiography during paced respiration is studied to evaluate cardiac parasympathetic innervation. This test is often the first electrophysiologic abnormality in patients with diabetic neuropathy. The quantitative sudomotor axon reflex test detects postganglionic sudomotor abnormalities and is available in many laboratories. Guides to the evaluation and testing of patients with autonomic failure are presented in several excellent reviews.
Neuropathies are in part classified based on the abnormalities seen on NCS and EMG. Demyelination (uniform or segmental) and axonal loss in both sensory and motor fibers can be studied physiologically. The study of more than one limb is needed to determine if the process is focal or diffuse. Side-to-side comparison is also very useful, especially if one of the limbs is abnormal. Superimposed compressive mononeuropathies occur in patients with neuromuscular disease, so abnormalities in typical locations such as at the elbow or at the fibular head need to be evaluated fully. Testing one sensory and motor nerve in both an upper and lower extremity is a standard screen for neuropathy. This screen should always include symptomatic areas. Needle examination of a few muscles is important to rule out axonal injury because the motor NCS can be normal early in a motor axonopathy. The EMG study can also render information concerning the chronicity of the process. If a sensory nerve is needed for biopsy purposes, it may be helpful to pick a nerve that has an abnormal NCS response. Sural nerves are commonly biopsied. A sural nerve with an abnormal response is often a good biopsy choice. However, an unobtainable sural sensory response does not necessarily reflect a sural nerve that will be too badly injured to demonstrate pathologic abnormalities. If a neuropathy is studied within the first few days of symptom onset, NCSs may be normal and repeat studies may be necessary. Myopathies are also evaluated by EMG. Each study of a possible myopathy must begin with NCS to rule out a superimposed neuropathy because some diseases can cause both myopathy and neuropathy. These disorders include sarcoidosis, thyroid disease, alcohol toxicity, HIV-related disease and rheumatologic disorders. Also, some neuropathic disorders begin with proximal weakness and mimic a myopathy; examples are spinal muscular atrophy. porphyria, lead exposure, and occasional cases of Guillain-Barre syndrome. Needle examination in myopathies is helpful for two reasons. First, the pattern of abnormality may be helpful in narrowing the differential diagnosis. For instance, most inflammatory myopathies have markedly increased insertional and spontaneous activity. Some myopathies, such as polymyositis and inclusion body myositis, have MUPs with both myopathic and neuropathic features. Steroid myopathies often do not have spontaneous activity present, which differentiates them from inflammatory myopathies. Metabolic myopathies may have little or no EMG abnormalities. A typical screening examination for a myopathy would include EMG of both proximal and distal muscles in two limbs. Also, paraspinal muscles should be included as they may be the only muscles demonstrating spontaneous activity in several myopathies including polymyositis and acid maltase deficiency. Second, in myopathy, EMG may be used to aid in picking a muscle to biopsy. Biopsy of a clinically moderately involved muscle that has moderate EMG involvement on the contralateral side may increase the yield. Muscles should not be biopsied in a location near the needle examination because of the inflammatory reaction that may ensue, leading to confusion when evaluating the biopsy specimen. Suspected neuromuscular junction disease is studied first by a conventional myopathy screen (NCS plus EMG) to rule out an underlying neuropathic or myopathic abnormality. Further testing with repetitive nerve stimulation or single-fiber EMG is then performed in search of a primary defect of neuromuscular junction transmission.
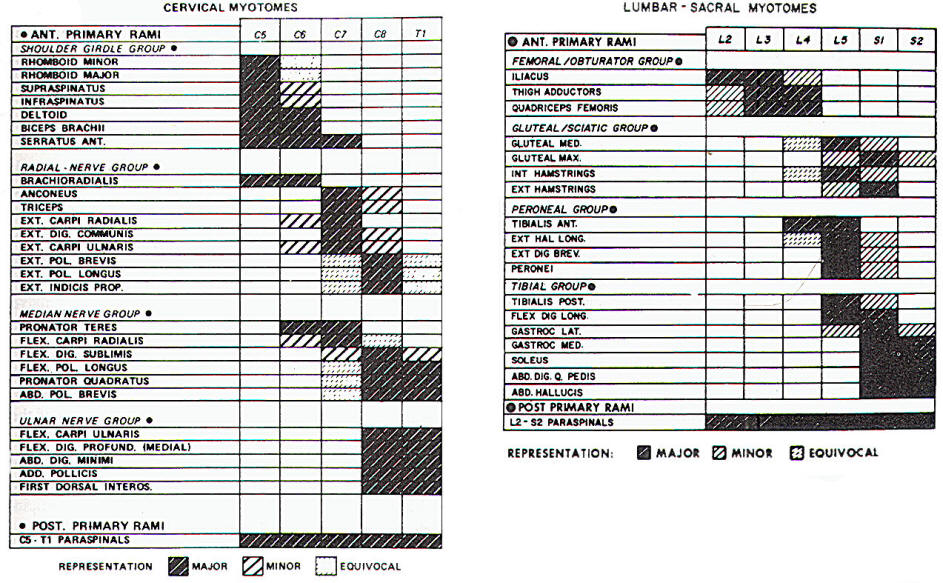
Electrophysiologic studies can be very useful in documenting the presence of a radiculopathy. However. a normal NCS/EMG study does not rule out the presence of a radiculopathy. When a patient with a radiculopathy is studied. a screening NCS is performed in the symptomatic limb to exclude a concurrent entrapment neuropathy such as a carpal tunnel syndrome or a more diffuse neuropathy. Although patients with radiculopathy may exhibit sensory loss clinically, sensory conductions should be normal because the cell body in the dorsal root ganglion is distal to the point of root injury. If the sensory response is abnormal, localization to a plexus or peripheral nerve is suggested. Motor conduction studies usually show normal distal latency and conduction velocity because stimulation sites are distal to the site of the lesion, Amplitudes usually do not drop with injury to one root because other roots are also innervating each muscle tested, Axonal injury in the root is seldom complete. With severe root injury as in multiple root avulsions or a cauda equina syndrome, amplitudes of the CMAP may diminish, F-wave latencies may be prolonged because of focal demyelination of the fast conducting motor fibers at the root level. Usually with a lesion of one root, however. other levels are sufficiently active to maintain a normal F-wave latency. Also, root injury may be focal, allowing some impulses to still get through. As mentioned, F-wave latencies can remain prolonged indefinitely after root injury. H-reflex testing may be useful in S1 radiculopathy. Unfortunately, as mentioned previously. many normal patients will have unobtainable H-reflexes and the H-reflex abnormalities can be present indefinitely after nerve injury, The advantage of the H-reflex is that it involves transmission along sensory and motor pathways. Needle examination is the most useful tool in evaluating radiculopathy, particularly if weakness exists, The most specific localizing finding is spontaneous activity in a myotomal distribution. A myotome is composed of muscles that have innervation contributed from the same root level. Neuropathic change of motor unit potentials may also be helpful but is less reliable for localization. After significant root injury, the first EMG change is delayed recruitment. Denervation changes may appear in a proximal to distal progression. Since the most proximal muscles are the paraspinal muscles, spontaneous activity may be seen within 1 week to 10 days in these muscles. Because of significant overlap in root innervation of paraspinal muscles. localization is imprecise. Needle examination of paraspinal muscles should therefore include several paraspinal levels above and below the site of presumed involvement to increase the yield. Within 2 weeks of significant root injury, spontaneous activity is commonly seen in paraspinal muscles and is often seen in proximal muscles. At 3 weeks distal muscles may also be involved. Motor unit instability can often be appreciated if active denervation changes are occurring and this may precede the formation of complex MUPs, Following resolution of the radiculopathy, denervation changes may disappear. However, since they sometimes persist to some degree indefinitely, a previous EMG study in an individual with a history of radiculopathy would be useful for comparison to be confident of an active ongoing process unless the findings are dramatic. Several muscles in the symptomatic limb that are innervated by different roots and nerves should be studied to search for a myotomal distribution of abnormality. Because of multiple root contribution to the innervation of a single muscle, it is often difficult to be certain about the localization of the radiculopathy. With post-EMG surgical correlation, it has been shown that common radiculopathies such as C6 and C7 radiculopathies cannot necessarily be distinguished by EMG. By utilizing standard references of muscle innervation, however, focal denervation in two to three muscles innervated by the same root and different nerves is suggestive of a radiculopathy at that root level (Fig-6). Not all muscles innervated by an individual root will necessarily show denervation changes. This is dependent on the time sequence of the EMG study relative to the onset of symptoms, the severity of the root lesion. and the variability of innervation patterns.
Focal paraspinal muscle abnormalities in EMG help to localize the lesion to the root level. Paraspinal muscles are innervated by dorsal rami. However, paraspinal muscles may not be involved if fibers to ventral rami are preferentially involved by root compression. If paraspinal muscles show an increase in spontaneous activity at multiple levels throughout the spine, other causes should be considered such as carcinomatous meningitis, polyradicular neuropathy, diabetic radiculopathy, or inflammatory myopathy. Abnormalities need to be bracketed by normal paraspinal EMG studies to ensure that a focal process is present. Paraspinal EMG examination can be abnormal up to 4 days following myelography so EMG studies should be done prior to myelography if needed. Also, paraspinal muscles may be abnormal indefinitely in a region of previous back surgery so abnormalities in this situation need to be interpreted with caution. The causes of paraspinal and limb radicular abnormalities by EMG are not determined by the study. Compressive or noncompressive causes such as diabetic radiculopathy or herpes zoster may be present. If diffuse EMG abnormalities are encountered in one limb, the contralateral limb should be studied. If that limb is abnormal, studies should proceed to the second limb to evaluate the possibility of a more diffuse process such as a neuropathy or motor neuron disease. Bilateral leg involvement is common in radiculopathy even in an asymptomatic limb. Conus medullaris lesions, a cauda equina syndrome or spinal stenosis often leads to bilateral, asymmetric electrophysiologic findings. If lower sacral roots need to be studied, sphincter EMG can be performed. In the upper extremity, a common problem is evaluating a traumatic injury. With significant trauma, denervation changes are seen in weak muscles and activation of MUPs imply nerve continuity to that muscle. If root avulsion alone is present, sensory NCS values are normal. However, coexistent plexus injury often occurs, resulting in abnormal sensory NCS values. In the lower extremity, diagnostic evaluation of foot drop is very common. Differentiating peroneal neuropathy from L5 radiculopathy is done by study of peroneal motor and sensory conduction and EMG study of L5-innervated muscles inside and outside of the distribution of the peroneal nerve. These muscles include the gluteus medius, short head of the biceps femoris, and tibialis posterior. Needle examination of the extensor digitorum brevis and abductor hallucis should be interpreted with caution because of frequent trauma to these muscles and the finding of abnormalities in patients who are normal clinically. Thus, NCS/EMG is useful in an evaluation of radiculopathy because studies will detect other causes of limb numbness and weakness, such as entrapment neuropathy or diffuse neuropathy, and can often document the radicular pattern of denervation. Studies may be less useful in patients with pure sensory complaints or a recent onset of injury. The sensitivity is similar to that of myelography. It must be recognized that asymptomatic subjects with a normal neurological examination can have EMG evidence of radiculopathy so these findings must be correlated with the clinical history and physical examination.
Plexopathies cause focal neurological dysfunction and are often divided into traumatic and non traumatic causes. Common nontraumatic causes of plexopathy include neuralgic amyotrophy (Parsonage- Turner syndrome), plexopathy due to tumor invasion, radiation-induced plexopathy, and diabetic amyotrophy. Sensory conductions are useful in plexopathy localization because the dorsal root ganglia are proximal to plexus lesions, resulting in abnormal sensory responses, most often a low SNAP amplitude. Motor conduction studies are less helpful in differentiating radiculopathy from plexopathy because they are usually normal. With multiple root or severe plexus injury, CMAP amplitudes may diminish as a result of axonal dropout. Similarly, if fast conducting fibers are interrupted, F-wave latency may be prolonged in either localization. The distribution of EMG abnormalities is an important factor in localizing the lesion to the plexus. Paraspinal muscle abnormalities suggest root involvement and are absent in plexus disease. The limb pattern of denervation changes is helpful for plexus localization. A typical example would be deltoid, triceps, and extensor digitorum communis muscle denervation with sparing of the biceps and spinati from a posterior cord lesion of the brachial plexus. The NCS/EMG study may localize the lesion to a plexus but cannot define the etiology. Specific findings, however, may be suggestive of a specific etiology. The Parsonage-Turner syndrome can affect a single root, trunk, cord, or nerve. One-third to one-half of patients may have bilateral symptoms and as many as one-half will have bilateral EMG abnormalities. Thus, if the Parsonage- Turner syndrome is suggested clinically, bilateral upper limb EMG should be performed even if one limb is asymptomatic, Lesions may also be patchy within the brachial plexus in this disorder. Myokymic discharges are suggestive of radiation-induced injury as opposed to tumor infiltration.' Diabetic amyotrophy is suspected in a diabetic patient with a typical history; the NCS/EMG study usually documents concurrent radiculopathy and neuropathy making localization to the lumbosacral plexus difficult. Spontaneous activity is often prominent in the proximal muscles involved but precise localization by EMG is unlikely in these patients because of their underlying neuropathic changes. Since etiology cannot be determined despite localization to the plexus, a clinical decision needs to be made concerning the use of neuroimaging studies to rule out tumorous involvement. The thoracic outlet syndrome (TOS) constitutes a specific type of brachial plexopathy that merits separate mention. It is best divided into true neurogenic TOS and disputed or non-neurogenic TOS. In neurogenic TOS the patient complains of paresthesias of the medial arm, forearm or hand and has weakness and atrophy of median - greater than ulnar-innervated muscles in the hand. This is due to compression of the distal C8 and T1 roots or the lower trunk of the brachial plexus. The pattern of the nerve conduction abnormalities in this type of TOS is characteristic. Because median nerve sensory fibers travel through the C5 and C6 roots and the upper trunk of the brachial plexus. the median sensory responses in the hand are normal. Ulnar sensory responses in the hand are abnormal (low amplitudes) because these fibers arc compressed proximally. Motor fibers to the median-innervated hand muscles do run through the C8 and T1 roots and the lower trunk so the CMAP amplitudes recorded from the abductor pollicis brevis are low and EMG of that muscle shows chronic denervation changes. The ulnar motor study may show low or low -normal CMAP amplitudes, and chronic denervation changes may be seen in the first dorsal interosseus muscle. Because the process is slowly progressive, prominent spontaneous activity may be absent. Patients with non-neurogenic TOS haw a normal neurological and electrophysiologic examination.
Peripheral nerves can be studied by both NCS and EMG in the evaluation of mononeuropathies. Discussion will be limited to the most common mononeuropathies evaluated by the neurosurgeon. Motor conduction studies of the facial nerve are obtained by stimulating the facial nerve as it exits the stylomastoid foramen under the ear while recording with a surface electrode over a facial muscle, usually the orbicularis oculi. Motor NCSs are particularly useful prognostically in patients with Bell's palsy. if CMAP amplitudes are compared between sides 1 to 2 weeks after the onset. In patients in whom the amplitude on the symptomatic side is less than 10 percent of that on the normal side, 79 percent will have incomplete recovery. More than 90 percent of patients will have a good recovery if the amplitude is greater than 10 percent of that on the normal side. The drop in amplitude is reflective of axonal loss in most cases. Some patients with Bells palsy can have a neurapraxic injury without a drop in amplitude: their prognosis for early recovery is excellent as the conduction block resolves. Because the facial nerve is usually injured along its path in the temporal bone. NCS during the first days of Bell's palsy will not be helpful in localization. Blink reflexes can be used to demonstrate a peripheral seventh nerve lesion with prolongation or absence of ipsilateral R1 and R2 responses. If the R1 response is present or returns early in the course of Bell's palsy, the prognosis is good. EMG is an important tool in the evaluation of facial nerve palsies because axonal loss may not necessarily affect the CMAP amplitude. The needle examination can help assess the degree of axonal injury and also be used to follow reinnervation. If no movement of facial muscles is seen clinically, and nerve grafting is being considered. EMG of several facial muscles can be helpful to look for the presence of voluntary motor units that would suggest that nerve continuity exists to those muscles. EMG change over time would help determine if reinnervation is occurring. Electrophysiologic study of diaphragm function is important in patients with unilateral or bilateral diaphragm weakness and in patients who are difficult to wean from a ventilator. Frequently, patients who cannot be weaned may have concurrent, unsuspected neuromuscular disease. Also, several neuromuscular diseases may affect the diaphragm and respiratory muscles early in the course of the disease. These include myotonic dystrophy, acid maltase deficiency and motor neuron disease. Initially, a screening extremity study should be done to rule out an underlying neuropathy or myopathy. If this study is abnormal, specific study of the diaphragm may not be needed. Phrenic nerve conduction studies can be done by stimulating the phrenic nerve superficially behind the sternocleidomastoid muscle and recording from the diaphragm with a surface electrode in one of several locations. The draw backs to this method are due to the technical demands of the study, especially when performed in an intensive care unit. and the low amplitudes of the CMAP recorded from a normal diaphragm. Thus, significant neuropathic or myopathic involvement can be present with relativey normal motor conduction studies of the phrenic nerve. Direct needle examination of the diaphragm is of more utility. This can be done safely even if the patient is on a ventilator. Special care is needed to avoid pulmonary structures in patients with chronic obstructive lung disease because their diaphragms are often more caudal in location than normal. The needle electrode is inserted through the superficial muscles and localization is proven by respiratory variation in diaphragm firing. It is not uncommon for active motor units to be found in diaphragms that were believed paralyzed on radiologic study. The needle examination can quantitate the degree of denervation. Myopathic abnormalities may be more difficult to recognize in the diaphragm because normal MUPs appear somewhat myopathic in this muscle. The presence of motor units with respiratory variation tells the neurosurgeon that phrenic nerve continuity exists and, especially after trauma, that recovery may ensue. Reinnervation of the diaphragm can be followed by serial studies. The most common median neuropathy referred to the EMG laboratory is the carpal tunnel syndrome. There are several different methods used to study the median nerve distally. Most commonly performed is an orthodromic study with stimulation in the palm and recording at the wrist with surface electrodes. Sensory conduction is usually the first parameter to be abnormal in the carpal tunnel syndrome. Prolongation of the distal latency occurs early because of focal demyelination of the median nerve in the tunnel. If digit-to-wrist studies are done, the distal latency may seem more normal because the focal conduction abnormality is averaged out over a longer distance. Both median nerves should be studied if a carpal tunnel syndrome is suspected because bilateral occurrence is present in up to 55 percent of patients, usually more severe in the dominant hand. In addition to using normal value, of median sensory nerve conduction for the determination of abnormality, asymmetry between sides and comparison to ulnar sensory response, is often useful. A 0.5-ms difference in distal latency at a stimulation to recording distance of 8 cm is a significant asymmetry between ipsilateral median and ulnar recordings. If digital stimulation is done. a middle finger study may be more sensitive than a ring finger study. Early motor conduction studies may be normal or show a slightly prolonged distal latency. As denervation changes occur, the CMAP amplitude will decline, signifying axonal dropout. F-wave latencies may also become prolonged. Sometimes EMG of median-innervated hand muscles is useful to document the presence of axonal injury, motor conduction studies can be normal in the face of active denervation changes in the hand. Examination of the abductor pollicis brevis should be done first and, if normal, the opponens pollicis should be examined. This study may influence the level of aggressiveness toward a surgical approach, especially if the abnormalities by NCS/EMG are seen to progress over time. Conventional NCS can be normal even if a carpal tunnel syndrome is present. A median nerve mapping study (inching) may be useful in the event that the study is normal and a carpal tunnel syndrome is highly suspected. A routine study for the carpal tunnel syndrome should also include ulnar motor and sensory studies to evaluate for a more diffuse neuropathy, and an EMG study, if neck pain is present. to rule out a cervical radiculopathy. If median nerve involvement more proximally is considered, needle examination of the pronator teres, flexor carpi radialis, or muscles in the distribution of the anterior interosseus nerve will aid in localization. In an anterior interosseus neuropathy, denervation changes are present only in the muscles innervated by that nerve branch, and median motor and sensory studies in the hand are normal. Ulnar nerve studies can be very useful in localizing lesions along the course of the nerve. Sensory responses from distal palmar stimulation test the superficial sensory branch, which passes through Guyon's canal. Digital testing, however, involves the dorsal cutaneous branch, which originates before Guyon's canal and would be spared by a lesion in the canal. When ulnar motor studies are performed, the elbow must be flexed (usually greater than 90 degrees) to ensure that the ulnar nerve is taut. Stimulation above and below the elbow at the ulnar groove, in addition to stimulation at the wrist, helps localize the region of conduction block by a significant drop in amplitude (conduction failure), a dispersed CMAP waveform, or a drop in conduction velocity. It is often difficult to differentiate between retrocondylar compression and cubital tunnel involvement. Stimulating short segments in 1-cm intervals above and below the ulnar groove may help demonstrate a conduction blocks. If a CMAP amplitude from proximal ulnar stimulation is significantly diminished from that achieved with distal stimulation, one must be sure a Martin-Gruber anastamosis (a normal variant) is not present. The most common type of this anastamosis involves ulnar fibers traveling with the median nerve proximally and joining the ulnar nerve in the forearm, resulting in a significantly higher CMAP amplitude with distal stimulation of the ulnar nerve. Median nerve stimulation proximally with recording from the abductor digiti quinti can demonstrate this cross-over. The flexor carpi ulnaris and flexor digitorum profundus arise in the forearm and usually are involved by EMG in very proximal ulnar nerve lesions. Nerve twigs to both of these muscles take off from the ulnar nerve distal to the cubital tunnel. Unfortunately, nerve fascicles to these forearm muscles can be spared in compression at the elbow, especially if neurapraxia predominates. Hypothenar and intrinsic hand muscles are innervated by the ulnar nerve after it travels through Guyon's canal and both should be involved with compression at the canal. Hypothenar muscles may be spared if compression occurs in the palm. Motor and sensory conduction studies of the median nerve are needed to rule out neuropathy and EMG of other muscles in the extremity should be done to rule out C8-T1 radiculopathy or a more diffuse denervating process. Localization of a radial neuropathy is aided by study of the superficial radial nerve response. This nerve originates proximal to the posterior interosseus nerve takeoff and is spared in posterior interosseus neuropathy but is involved in proximal radial nerve lesions. By EMG the triceps muscle is usually spared in radial nerve compression at the humeral groove while muscles from the brachioradialis distally are involved. Posterior interosseus entrapment at the arcade of Frohse will spare the extensor carpi radialis longus and brevis because nerve twigs to these muscles exit the radial nerve proximal to the arcade. Superficial peroneal sensory conduction studies are frequently abnormal in common or superficial peroneal neuropathy. Motor studies are usually recorded from the extensor digitorum brevis after stimulation at the ankle, below the knee, and above the knee. If a focal conduction block is not found by a drop in conduction velocity or amplitude across a segment of the peroneal nerve (usually at the fibular head), inching studies can be performed across the fibular head if compression is suspected or better localization of the block is needed. If the extensor digitorum brevis is severely atrophic, motor conduction studies can be done by recording from the anterior tibialis muscle. F-wave prolongation can occur with an abnormality anywhere along the peroneal nerve or more proximal fibers, so it is relatively non localizing if the peripheral conduction is abnormal, Needle examination is used to differentiate among L5 radiculopathy, plexopathy and mononeuropathy. The short head of the biceps femoris muscle is innervated by the peroneal trunk of the sciatic nerve and will often be involved in an L5 radiculopathy or lumbosacral plexus lesion. It should, however, be spared if peroneal compression occurs at the fibular head. Common peroneal, superficial peroneal and deep peroneal neuropathies are further defined by needle examination of the muscles innervated by those nerves. The extensor digitorum brevis (EDB) is a relatively unreliable muscle to study because denervation changes may be present in normal subjects. Therefore, isolated denervation changes in that muscle, or low CMAP amplitudes on the peroneal motor conduction study recorded from the EDB without denervation changes in other muscles supplied by the peroneal nerve or L5 root need to be interpreted with caution. If peroneal studies are abnormal, tibial motor and sural sensory studies should be performed in addition to contralateral studies to evaluate for lumbosacral plexopathy, a cauda equina syndrome or a more diffuse neuropathic process. The most common tibial distribution entrapment is the tarsal tunnel syndrome. Patients can be evaluated by NCS/EMG, but this is often difficult technically. Sensory responses from medial and lateral plantar nerves are obtained with orthodromic surface stimulation at the plantar surface and recording from the tibial nerve proximal to the tunnel at the ankle. Comparison of the symptomatic to the asymptomatic side is an important control, Because this study can be technically difficult, an absent plantar SNAP is often of uncertain significance. When the response has a prolonged distal latency. especially if it is asymmetric with the contralateral side, there is more confidence in diagnosing nerve entrapment. A study in which small needle electrodes are placed near the plantar nerves ("near nerve recording") may be more sensitive in detecting a conduction block. Patients often tolerate this procedure poorly. If responses are found to be abnormal, further NCS should ensue to rule out a diffuse peripheral neuropathy. In the setting of a diffuse peripheral neuropathy it is difficult to diagnose this syndrome with an electrophysiologic study. Motor conduction studies may show a prolonged distal latency when recording is performed from the abductor hallucis muscle and the tibial nerve is stimulated. Once again, EMG abnormalities in the abductor hallucis muscle may be unreliable because abnormalities in that muscle are seen in normal subjects. Needle examinations of the hamstring, gastrocnemius and soleus muscles are also used to search for a more proximal tibial nerve lesion. A follow-up conduction study can document improvement after tarsal tunnel surgery.
NCS and EMG can be very useful as operative monitoring tools. Facial nerve studies prior to acoustic neuroma surgery can help in assessing the degree of facial nerve involvement and predicting the prognosis for facial nerve recovery. If moderate or severe neuropathic findings are found by NCS/EMG preoperatively, the likelihood of full recovery postoperatively is poor. Intraoperative recording can be helpful in several ways. Neurotonic discharges, which are bursts of high-frequency discharges, recorded from a needle electrode in a facial muscle occur after nerve irritation. This can allow instant feedback to the neurosurgeon if on audio. The facial nerve or suspected facial nerve fibers can be stimulated in the operative field with recording from a facial muscle either by a surface or needle electrode to determine if the fibers are in fact facial nerve and if nerve continuity exists. . Facial nerve studies may be helpful in surgery for hemifacial spasm (HFS). In patients with HFS, either stimulation of the supraorbital nerve during a blink response or direct stimulation of a motor nerve can result in a response in muscles innervated by branches of the facial nerve other than that stimulated. This "lateral spread" is due to ephaptic transmission at the site of facial nerve cornpression. Intraoperatively. facial muscles can be monitored for neurotonic discharges during surgery for HFS. Intraoperative disappearance of the lateral spread response correlates highly with resolution of the HFS, while persistence of this response during surgery carries a poor prognosis for complete recovery. Thus, further search for compressive vessel is suggested if the lateral spread response persists. When peripheral nerves in the limbs are being operated upon, EMG monitoring with needle electrodes in appropriate muscles can be used to listen for neurotonic discharges. Also, motor or sensory nerve recordings from a nerve stimulated at the operative site can ensure continuity and sometimes assist with localization of a conduction block. The best example is ulnar stimulation after flexor carpi ulnaris division to determine if a conduction block is localized to the forearm or is present at the elbow. If the conduction block was localized to the forearm, cubital tunnel release is done without nerve transposition. If the conduction block was proximal to the medial epicondyle, transposition out of the ulnar groove is performed. Needle recording from the anal sphincter can be useful in surgery for a tethered spinal cord. Monitoring for neurotonic discharges and stimulation studies may help the surgeon avoid transecting roots. Finally, intraoperative monitoring is used by some during selective dorsal rhizotomy. Pathologic rootlets are thought to contribute to excitatory input of motor fibers. By stimulating portions of the dorsal root and evaluating which root fascicles cause contraction in multiple muscles or a high degree of contraction in individual muscles, roots are sectioned selectively, leaving some of the root at each level intact to preserve sensory function. However, it remains uncertain that intraoperative monitoring improves the results over those achieved by random root sectioning. Operative monitoring is technically demanding because of multiple potential sources of electrical interference and because of temperature considerations. Also, neuromuscular junction blocking agents cannot be used fully during the operation, although they may be used for intubation.
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|